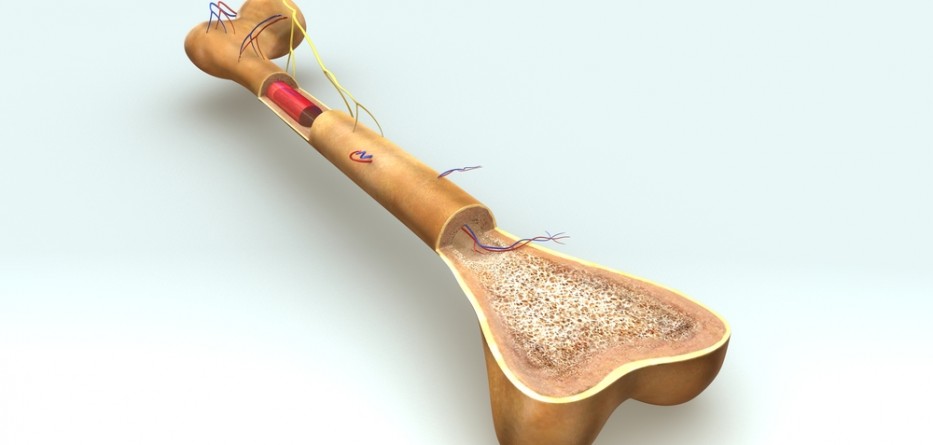
When a patient is diagnosed with multiple myeloma, their healthcare team goes through all therapy options with them depending on their particular case. There are mainly two approaches to the treatment of multiple myeloma: local therapies or systemic medications.
Local therapies such as radiation therapy or surgery entail targeting the cancer mass without invading any other part of the body. In most cases, these options are viable for those whose multiple myeloma is in its early stages.
Multiple myeloma may also be treated with systemic medications, taken either orally or intravenously. Systemic drugs are able to target myeloma cells throughout the body. The standard systemic medications used in the treatment of multiple myeloma include chemotherapy medications, stem cell transplant, bisphosphonates, or plasmapheresis. Some patients may also require a combination therapy consisting of different treatment methods.
Immunomodulators
Three medications classified as immunomodulators are typically prescribed for the treatment of multiple myeloma. The first immunomodulator that was ever designed was , which was associated with serious birth defects if used during pregnancy. Most immunomodulating drugs are also prescribed in conjunction with a blood thinner as they are associated with an increased risk of blood clot formation.
for Multiple Myeloma Treatment
Developed by Celgene, is a descendant of . Classified as an immunomodulator, similar to , inhibits the growth cancer blood vessels.
The FDA approved in February 2013 to be used as a form of treatment for those with relapsed or refractory multiple myeloma. Moreover, the medication can also be used as a treatment in patients with a history of a minimum of two courses of therapy consisting of and whose disease advanced within two months upon the conclusion of their treatment. is typically used in conjunction with a low dose of .
The only side effects of are a decrease in the count of red blood and white blood cells. is linked to a lower risk of nerve damage compared to its counterparts but can also put one at a higher risk of blood clotting.
Featured Image: DepositPhotos@sciencepics